Module 5 Libre : Vivre avec le VIH
Module 5:
Contents
LEARNING OBJECTIVES
At the end of this module, the participant will be able toDIAGNOSIS
Unlike the 1990s, when being diagnosed as HIV-positive was too often synonymous with a death sentence, in the 21st century, thanks to scientific and medical progress and advancements in HIV treatments, people living with HIV have a life expectancy and quality of life equivalent to those who are HIV-negative.
Thanks to increasingly effective testing and treatment, HIV is now considered a chronic disease and does not prevent people from living an altogether normal life:
.


.


.


HIV-POSITIVE. NOW WHAT?
Once diagnosed as being HIV-positive, the person is treated by a doctor (in Luxembourg, the reference service is the Service National des Maladies Infectieuses at the CHL) who will prescribe an antiretroviral treatment adapted to the infection. This treatment, generally consisting of one tablet to be taken once a day, will prevent the virus from reproducing and will reduce the viral load within a few weeks or months.
This means that the amount of virus in the blood will be so reduced by the treatment that it will no longer be detectable! This scientific breakthrough has led to the concept of U=U, i.e. Undetectable=Untransmissible, which entails that:
The immune system of people who are HIV-positive can be preserved (if the HIV infection is detected early) or restored, thereby ensuring sound health and avoiding the AIDS stage.
A person living with HIV under regular and effective antiretroviral treatment, with an undetectable viral load for at least six months, cannot transmit sexually.
The risk of transmission from mother to child during pregnancy and childbirth is 1% or close to zero.
An HIV-positive person who takes his or her treatment correctly and has an undetectable viral load therefore no longer transmits HIV!
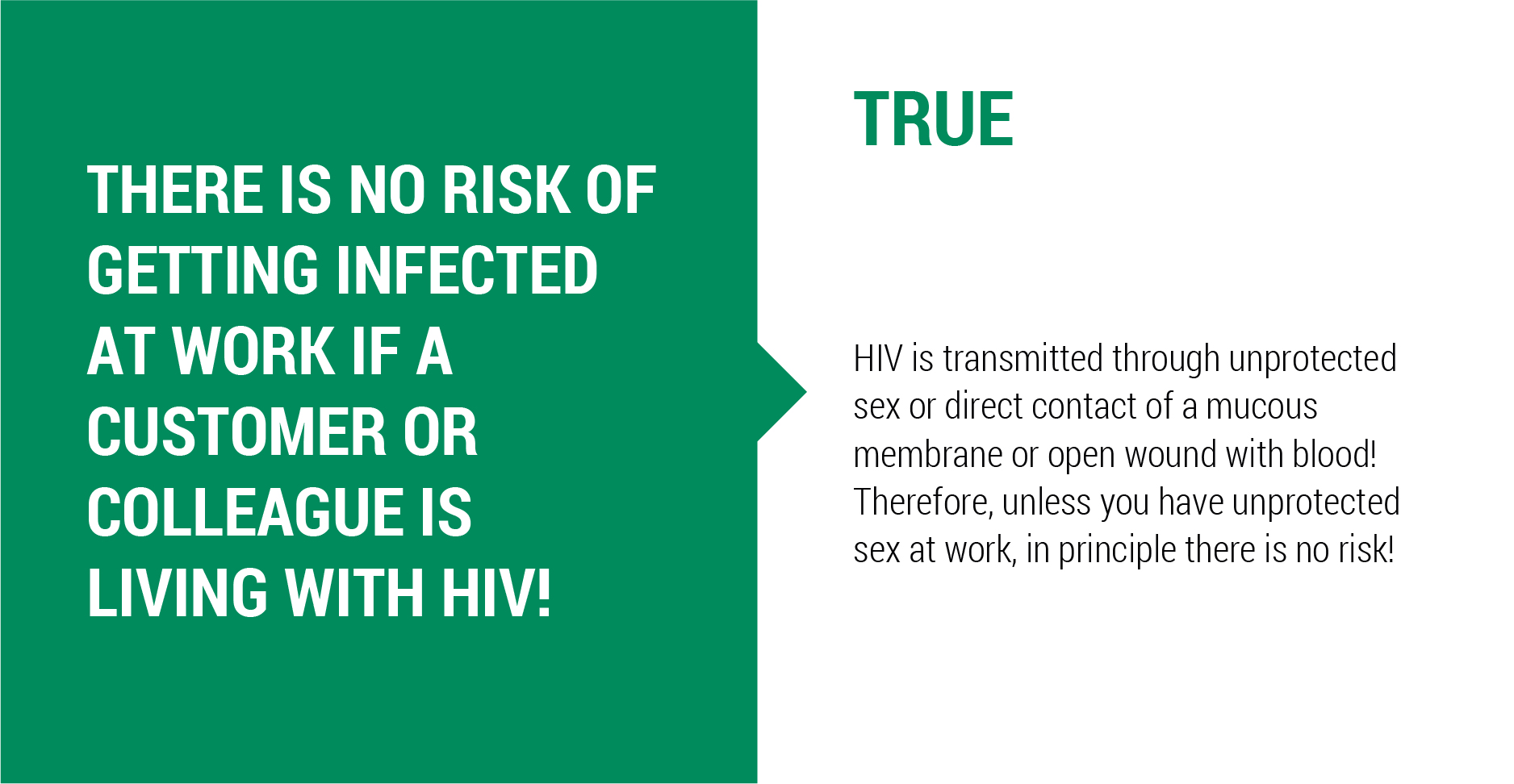
Reminder: an HIV-positive person does not entail any specific risks to those around him or her by sharing their day-to-day life. Eating together, using the same dishes, sharing the same toilet, bathroom, kissing, touching and even having sex (provided you are undetectable) do not carry any risk of transmission!
Regular medical check-ups are still necessary to monitor whether the virus in the blood remains undetectable and to screen for other potential sexually transmitted infections (STIs).
The use of condoms remains the most effective way to protect against STIs and is also a means of contraception.
The medical reference service specialising in all matters relating to HIV and treatment is the Service National des Maladies Infectieuses (SNMI) of the Centre Hospitalier du Luxembourg (CHL).
WHO WILL TAKE CARE OF THE TREATMENT?
An HIV infection does not affect the affiliation to health, pension and dependency insurance. In Luxembourg, the Caisse National de Santé (CNS) finances antiretroviral drugs fully (100%).
Luxembourg residents who are diagnosed as HIV-positive and are not affiliated to a health insurance fund can contact the HIV Berodung service of the Luxembourg Red Cross, which will take the necessary steps to make sure that the person gets access to treatment.
WHO TO TELL? AND HOW?

Tell partner(s), family, friends, colleagues, children? This is a recurring question among people living with HIV. Do they have to tell? Do they want to tell? Can they say it without fear of repercussions?
Whether or not to tell is a very personal and individual choice. Under no circumstances, is the person obliged to tell, be it to family, employer, colleagues or even sexual partner. Talking about it can be a relief: being able to share your fears and anxieties about the infection can be comforting.
Unfortunately, it is still too often the case that people who have learned of their son's, daughter's, friend's or colleague's HIV-positive status react negatively, cut ties with the person concerned, or even resort to defamatory and/or discriminatory comments or actions.
There is still a lot of misconception, stigmatization and discrimination around HIV.
Fortunately, many HIV-positive people have had wonderful experiences when they informed others of their HIV status! To fight against the discrimination that still persists, it is important to talk about HIV, to increase people's knowledge so that they are no longer afraid! Because it is often the fear of the unknown that fuels a discriminatory attitude.
If a person living with HIV has doubts or fears about the reaction of others, it is always good to talk about it first with people who are close to him or her and whose reactions can be more easily anticipated. Being well informed about the modes of transmission and existing treatments will enable the HIV-positive person to answer the questions of those around him or her, and thus dispel fears, prejudices and false beliefs.
It is always possible to contact the HIV Berodung service for advice and/or to prepare the announcement with a professional.
Talking about one's HIV status with a partner or partners, especially if prevention is guaranteed, remains a personal choice. With a life partner, it may be difficult to keep one's HIV status secret and this could be a burden on the relationship. On the other hand, the fact that the couple can talk openly about risks, fears and preferences, enables them to choose how to deal with the infection in their sexual life and how to ensure prevention.
The moment when the infection is announced is often moment for both of them. It is not uncommon for the partner to be afraid that he or she has also become infected or will become infected in the future. It is therefore useful to think about the questions that might arise and to inform oneself as much as possible before the discussion. The announcement of the result can also be prepared or done with the support of a professional from the HIV Berodung service of the Red Cross.
Being HIV-positive does not prevent a person from having sexual partners or a life partner.
He or she can use a prevention tool such as condoms or the HIV-negative partner(s) can use PrEP - Pre-Exposure Prophylaxis. It is recommended to start treatment in order to have an undetectable viral load and to stop transmitting HIV by sexual means. The treatment also ensures that the health of the HIV-positive person is preserved.
An effective means of prevention is TasP – Treatment as Prevention.
SHOULD YOU TELL YOUR EX-PARTNERS THAT YOU ARE HIV POSITIVE?
Even if it is not easy to do so, it has the major advantage of being able to encourage ex-partners to be tested, to know their HIV status and, if they are found to be HIV-positive, to get HIV treatment. It is advisable to discuss this with your doctor, who can advise and guide you in this process.
DESIRE FOR A CHILD
Having an HIV-negative child (i.e. one without HIV), without exposing the partner to risks, is nowadays possible for an HIV-positive person. Many people living with HIV have children.
An HIV-positive person on treatment with an undetectable viral load no longer transmits HIV through sexual intercourse - HIV-positive people can then become parents without fear of transmitting the virus to their partner.
Transmission of the virus from the HIV-positive pregnant person to the child during pregnancy and/or delivery can also be prevented through treatment. Antiretroviral treatment during pregnancy, delivery and the postnatal period can reduce the risk of HIV transmission to the child to less than 1%.

PREGNANCY
A person living with HIV can transmit the virus to her child during:
- pregnancy,
- childbirth,
- breastfeeding.
In the absence of treatment, the risk of transmitting HIV from a person to their baby is between 15-30%.
In Luxembourg, every pregnant person under gynaecological supervision is tested for HIV, syphilis, hepatitis C (and other diseases and infections) by means of a blood test. An HIV infection would thus be detected and the woman could receive antiretroviral treatment immediately.
With treatment in place, the risk of infection for the baby is reduced to less than 1% and a vaginal delivery also becomes possible.
If the viral load is too high, a caesarean section is recommended.
PROTECTING THE BABY DURING PREGNANCY:
When HIV is discovered BEFORE pregnancy


When HIV is discovered DURING pregnancy


In both cases, the baby will receive treatment (PEP, see Module 4) for a short period after birth to minimize the risk of transmission further and will be monitored during the first months of life.
BREASTFEEDING AND HIV?
Breastfeeding is currently still not recommended. Breast milk is one of the body fluids that can transmit HIV. New studies show that with an undetectable viral load, the risk of HIV transmission from the breastfeeding mother to her child is extremely low.
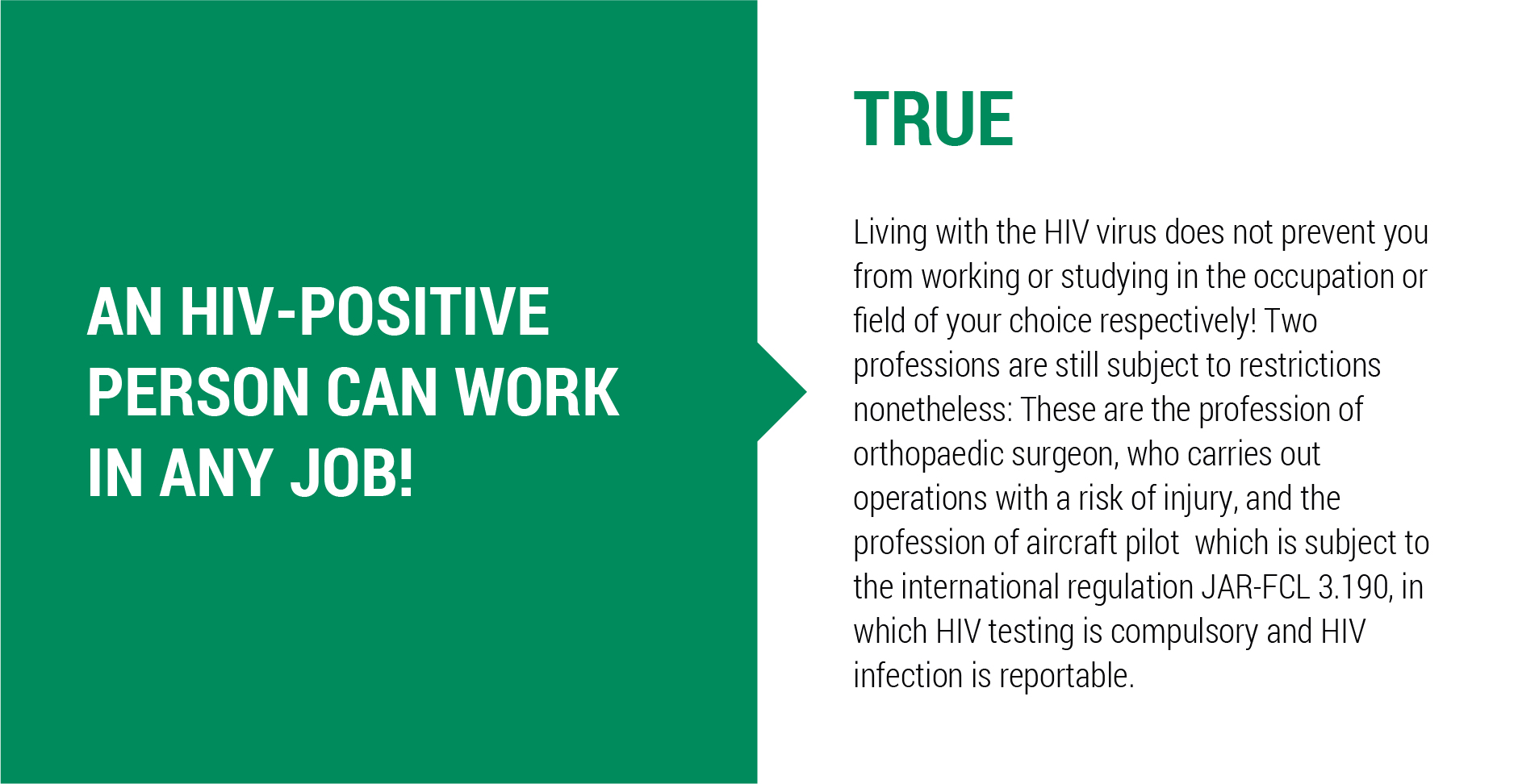
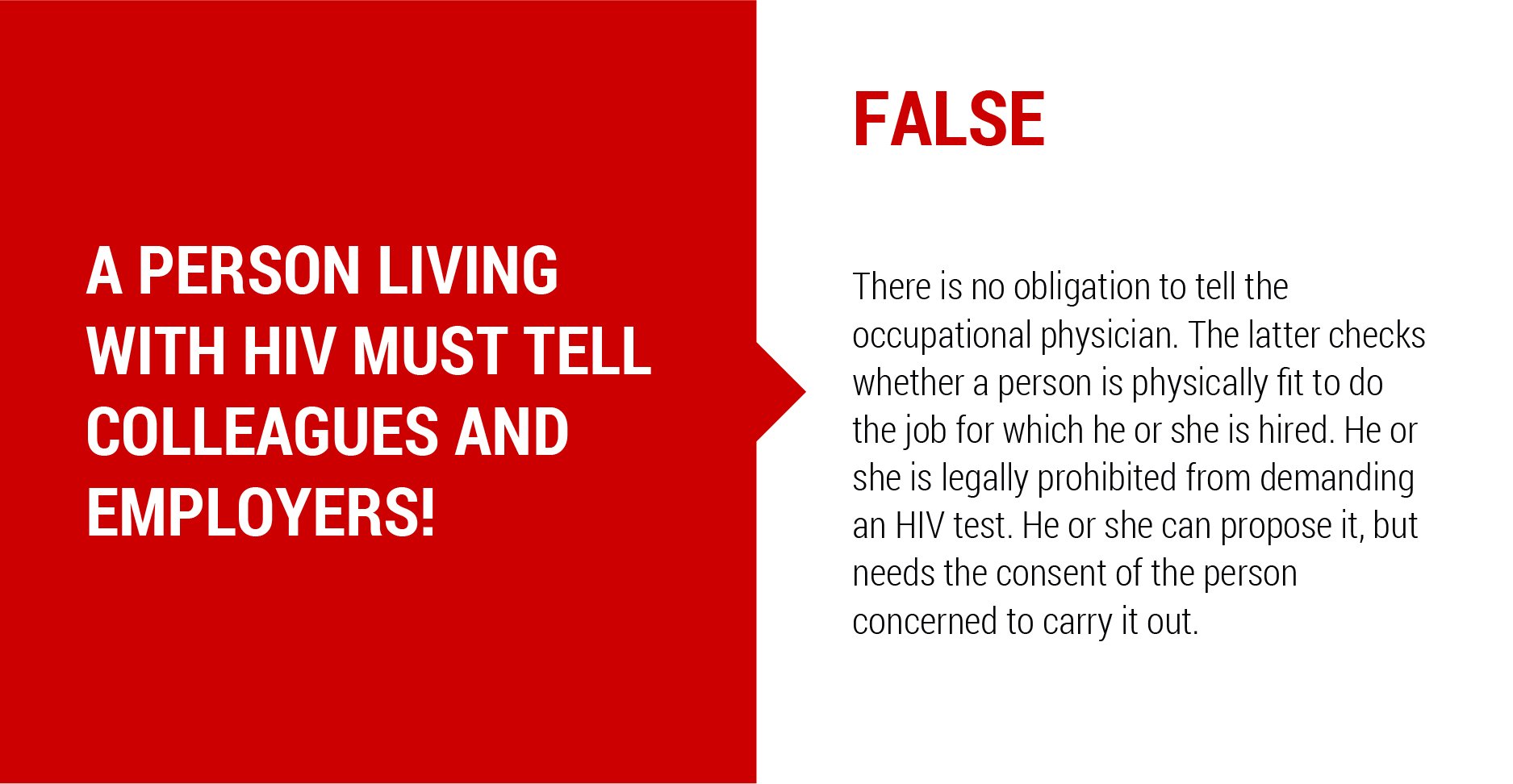
HIV STATUS AND WORK?






WHERE TO FIND SUPPORT?
HIV BERODUNG OF THE LUXEMBOURG RED CROSS:
- Advice and support for people and their entourage / family
- Psychological support for people who have just been diagnosed with HIV and/or are living with HIV and/or their families
- Social support for people living with HIV who have difficulty accessing treatment
- Information and advice
- Condoms
- Rapid screening tests
SERVICE NATIONAL DES MALADIES INFECTIEUSES (SNMI) OF THE CENTRE HOSPITALIER LUXEMBOURG (CHL):
- Information and advice
- Blood tests
- Medical care and treatment
- Prescription PrEP, PEP, TAsP
AIDS SURVEILLANCE COMMITTEE
The AIDS Surveillance Committee was established by ministerial order on 24 January 1984, following a recommendation by the World Health Organization on the proposal of the Director of Health.
In 2015, following a recommendation by the World Health Organization to create a multidisciplinary surveillance committee, the committee was reconstituted as the AIDS, Infectious Hepatitis and Sexually Transmitted Diseases Surveillance Committee.
The committee has the following tasks:
- Inform the general public, target groups and health professionals on all matters concerning AIDS, infectious hepatitis and sexually transmitted diseases
- Cooperate closely with national and international organizations to develop and implement programmes to combat AIDS, infectious hepatitis and sexually transmitted diseases
- Advise on all matters on public health relating to AIDS, infectious hepatitis and sexually transmitted diseases referred to it by the Minister
- Study and propose on one’s own initiative any measure or improvement in the field of prevention and control of AIDS, infectious hepatitis and sexually transmitted diseases.

