Module 4 Libre : Dépistage et prévention
Module 4:
Contents
LEARNING OBJECTIVES
At the end of Module 4, the participant will be able to:PREVENTION TOOLS
Protecting yourself and others has never been easier.

INTERNAL AND EXTERNAL CONDOM
SCREENING TEST
TAsP
PEP
PrEP
ROR
There is a range of prevention tools that may be more appropriate or preferred depending on the time or frequency of sexual practices.
SCREENING TEST
The HIV screening test is the only way to know one's HIV status and therefore to detect infection.There are many situations in life that may motivate people to take an HIV test:
- Following a risky situation (unprotected sex with a new or unknown partner; tearing, slipping of condom during sex; use of and/or pricking with a needle already used by another person)
- Before stopping using condoms
- When planning a pregnancy
- After a diagnosis of an STI, hepatitis (B or C) or tuberculosis
- After a sexual assault or rape
- Or simply when in doubt and in need of reassurance
The most important reason to get tested or to do so regularly when you are at risk of HIV transmission is that:
Getting tested = knowing your status = having access to treatment = undetectable viral load = maintaining your health and not transmitting HIV!
- The conventional blood tests: a blood sample is taken at the hospital or in a laboratory by a health professional, followed by a serological examination in the laboratory (e.g. Elisa test). Results are available after a few days.
- Rapid diagnostic tests (RDTs): a drop of blood is taken from a fingertip by a health professional (association or medical service) and mixed with a reagent. The result is available within 1 to 15 minutes.
- Self-tests: the collection, handling and reading of the result are carried out by the person himself or herself independently, for example at home. In Luxembourg, these tests can be bought in pharmacies or supermarkets (for purchases on the internet, please make sure the kits bear the CE marking). A result is visible after 15 to 20 minutes.
All these tests look for the presence of anti-HIV antibodies in the blood or the P24 antigen of the virus.
There are also tests that detect the virus directly (PCR test) or that can determine the viral load (amount of virus in the blood), but these are used only in very specific cases where a very early detection is needed (e.g. in the new-born of an HIV-positive mother or before using blood for a transfusion).
- Directly after infection, HIV multiplies unhindered and silently in the body. It cannot then be detected by any test. This is known as the window period.
- After about ten days, PCR tests can detect the virus in the blood.
- After about 2 weeks, the p24 antigen, an HIV protein, becomes detectable in the blood by a 4th generation combination test.
- After 2 to 5 weeks, anti-HIV antibodies, produced by the body's immune response, become detectable in the blood. This is the most commonly used method.
The window period is the time between when a person is exposed to HIV and when the virus can be detected in the blood. This is known as seroconversion. Seroconversion can vary from person to person and the detectability of HIV also depends on the test carried out (what the test detects). A certain period of time after the last risk situation must be observed for a reliable and safe result.
To confirm that there is no infection, you have to wait:
- 6 weeks after the risk situation for the blood test - antigen and antibody test
- 12 weeks (3 months) for the rapid diagnostic test (RDT) or self-test - antibody test
Until you have been tested and can rule out infection, you should always use a prevention tool (condom) and protect your partner(s)!
If the window period is respected, a negative test means that the person is HIV-negative and has not contracted HIV, but is not safe from future infection if he or she does not take protective measures.
If the test is positive, it means that the person is HIV-positive and therefore a carrier of HIV who can transmit the virus. A positive test will always be followed by a confirmation test and a blood test! In case of a positive result, medical follow-up and treatment can be started. In Luxembourg the specialised service is the Service National des Maladies Infectieuses --- You can't use shortcodes inside element ---.
!! IMPORTANT: HIV tests do not detect other sexually transmitted infections such as herpes, syphilis, chlamydia, gonorrhoea or viral hepatitis.
- The test is only compulsory in the case of blood, sperm or organ donation.
- It is systematically proposed to pregnant women.
- The classic blood tests (blood tests) proposed by a doctor do not include the HIV test. Contrary to popular belief, an HIV test will only be ordered at the explicit request or with the consent of the patient.
The conventional blood test is done in hospitals or laboratories. At the CHL, the Emile Mayrisch Hospital and the National Health Laboratory, they are free, anonymous and do not require a prescription.
RDTs are done at the HIV Berodung service of the Luxembourg Red Cross, in the DIMPS - the mobile screening unit, and at the LGBTIQ+ Cigale Centre. They are free, anonymous and do not require a prescription.
Self-test kits can be bought in pharmacies and supermarkets. There is also a free offer at the HIV berodung service of the Luxembourg Red Cross.
More information www.aids.lu and www.dimps.lu or call 2755 4500
TASP = TREATMENT AS PREVENTION
TasP (Treatment as Prevention) means that the treatment of an HIV-positive person becomes a means of prevention.
The aim of treatment is to reduce the viral load in the body so that it becomes undetectable and an HIV-positive person who has an undetectable viral load for 6 months on effective treatment and who complies with his or her treatment and medical follow-up no longer transmits the virus.
Thus, ARV treatment, which initially aimed to treat and improve the life expectancy and quality of life of people living with HIV, is also becoming a very effective means of prevention.

GOOD TO KNOW:
Undetectable = Untransmissible
PEP = Post exposure Prophylaxis
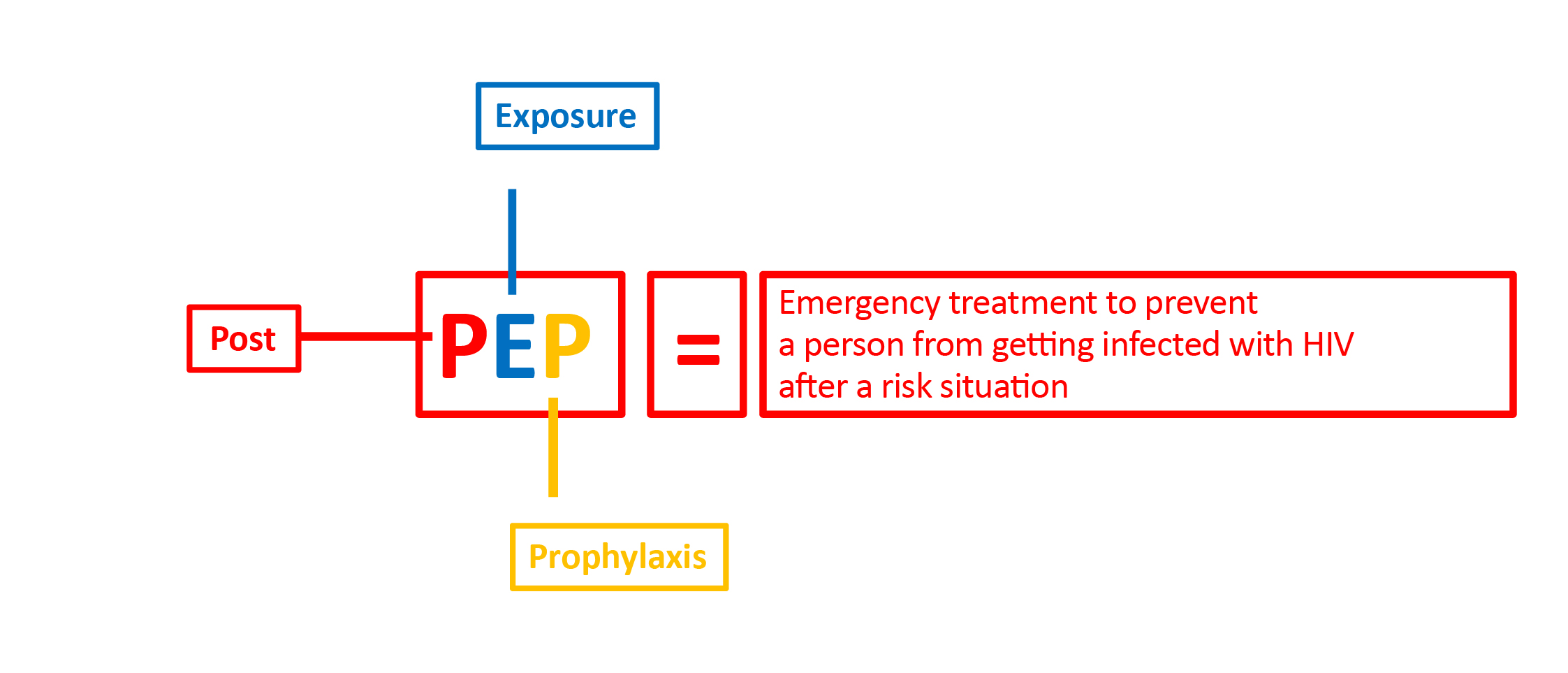
There is an emergency treatment, to be taken after a situation of risk of HIV infection.
This treatment is called PEP - Post-Exposure Prophylaxis.
The treatment generally consists of several drugs, triple therapy, and in this case aims to reduce the risk of HIV infection significantly by preventing the virus from entering the cell, replicating and spreading throughout the body.
Post-exposure prophylaxis should be started as soon as possible, preferably within 4 hours and ideally within 48 hours of a risk of HIV transmission.
After 48 hours it loses its effectiveness and after 72 hours it will no longer be effective and will no longer be prescribed.
The earlier the treatment is started, the more effective it will be!
- In the hours following exposure to HIV: go to the infectious diseases department of the Centre Hospitalier du Luxembourg (CHL) or to another emergency department as quickly as possible
- Ideally within 48 hours
- Imperatively within 72 hours
The medical staff on site will assess the risks of exposure and a preventive treatment may be prescribed, in order to avoid a possible infection by HIV.
PEP is an emergency treatment intended to reduce the risk of transmission of the virus after a risky situation such as:
- Unprotected vaginal or anal sex (breaking, slipping, misuse of condom)
- Rape or sexual assault
- Oral sex with ejaculation in the mouth
- Eye/mouth contact with contaminated semen or blood
- Accidental pricking with a used needle
- A blood exposure accident while under medical care (injury with a syringe)
- Sharing of used needles
- Prolonged blood contact with mucous membrane or injured skin
- Unprotected vaginal or anal sex with a person with a positive HIV status or belonging to a risk group*
- Sharing sex toys
You should go directly to the Infectious Disease Unit U20, on the 2nd floor to avoid wasting time in the emergency room.
A doctor will assess the risk situation with the patient and decide whether PEP is necessary.
If so, the treatment will be administered immediately for 3 days.
At the end of these 3 days, an HIV referral doctor will review the situation with the patient during a new medical visit: he or she may then decide to stop, change or continue the treatment for 28 days depending on several factors (tolerance, reassessment of risk, etc.).
For the treatment to be effective, it is essential to respect the duration, prescribed doses and times of intake!
A blood test after 1 month will determine whether an HIV infection has been prevented.
A second blood test after 3 months will screen for other infections such as syphilis and hepatitis C.
It is also available in the emergency services of the:
- Centre Hospitalier Emile Mayrisch at Esch/Alzette
- ZithaKlinik à Luxembourg-gare (Robert Schuman hospital group)
- Kirchberg Hospital
- Centre Hospitalier du Nord at Ettelbrück.
More about PEP
PrEP = Pre-Exposure Prophylaxis
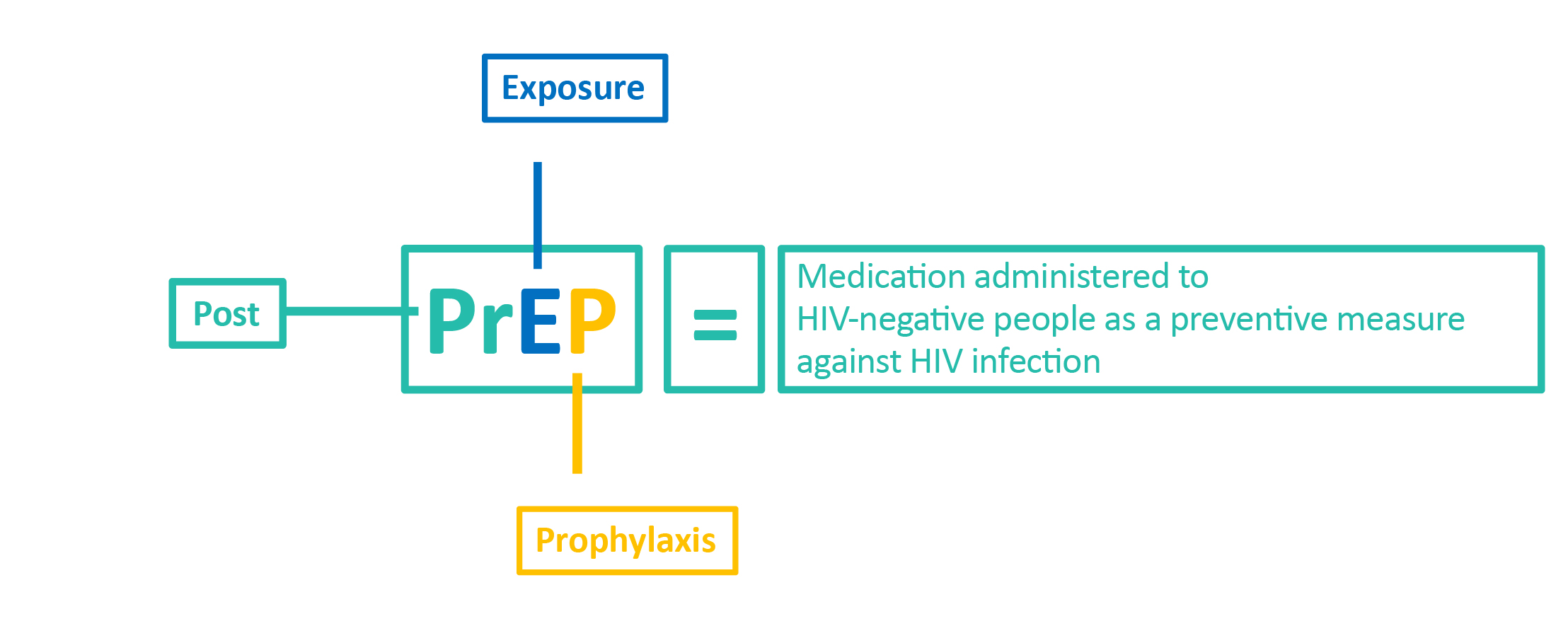
PrEP stands for PRE-EXPOSURE PROPHYLAXIS.
It is a preventive strategy to reduce the risk of contracting HIV by undergoing a treatment consisting of 2 antiretrovirals before the risk situation.
This prevention tool is recommended for HIV-negative people at high and repeated risk of HIV infection.
!! Attention: PrEP only reduces the risk of contracting HIV but does not protect against other sexually transmitted infections.
PrEP is available only by prescription from the Service National des Maladies Infectieuses of the CHL.
It requires regular medical follow-up and personalized sexual health support, including screening for other STIs.
continuous use, which means taking one antiretroviral tablet (Truvada®) a day
punctual use, which means taking two tablets two hours before taking a risk and one tablet 24 and 48 hours after taking a risk.
For PrEP to guarantee effective prevention, the medical prescription must be scrupulously adhered to.
PrEP is available: in Luxembourg, at the Service National des Maladies Infectieuses of the CHL, covered by the Caisse Nationale de Santé (CNS) --- You can't use shortcodes inside element ---. For a consultation with a view to obtaining PrEP, it is necessary to contact the Service National des Maladies Infectieuses of the CHL at +352 4411 3091.
More about PREP
CONDOMS – DENTAL DAM
Internal and external condom
The condom is the only tool that protects against HIV, other STIs and unwanted pregnancy.
How do you put on an internal (female) condom?
First, check the expiry date, the CE marking, and whether there is air in the package.
As with the male condom, avoid storing female condoms in your purse or wallet (friction damages the condom) and in the car or near a heat source (heat dries out the condom and makes it more fragile).
Wash your hands preferably before opening the package and get into a comfortable position: lying down, sitting or squatting as if putting on a tampon.

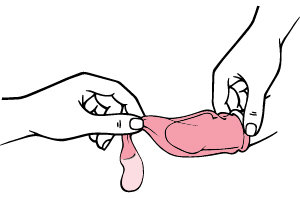
How to open a packaging correctly?

How to put the condom on?
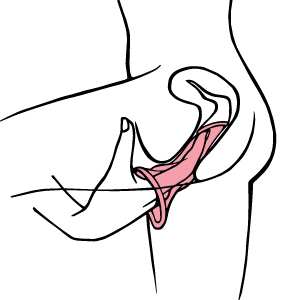
How to put the condom on? (continued)
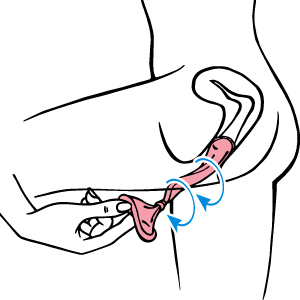
How to take the condom off?
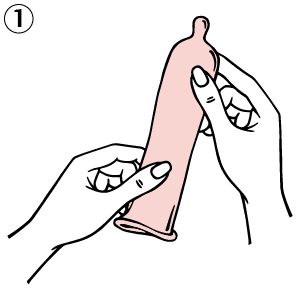
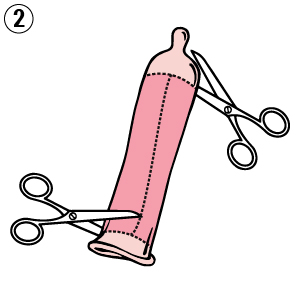
How to put a male condom on?
Avoid storing condoms in your purse or wallet (friction damages the condom) and in the car or near a heat source (heat dries out the condom and makes it more fragile).
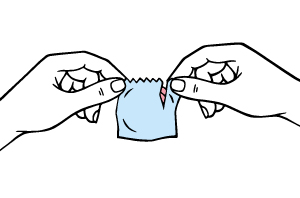
How to open a package correctly?
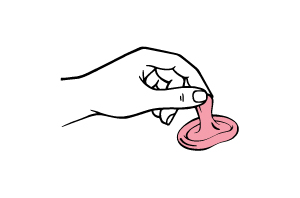
Direction of the condom
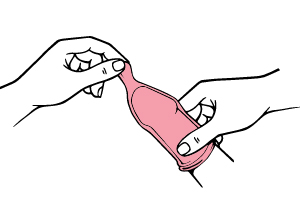
How to put the condom on?
How to take it off?
Where to put it once removed?
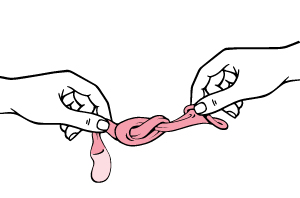
Dental dam:
How to put it on?
Where to buy it?

How to make a dental dam from latex?
ROR = REDUCTION OF RISK

Using drugs (on an experimental, recreational, occasional, abusive or addictive basis) can have an effect on physical health (e.g. injuries, thrombosis, infections including HIV and HCV, respiratory depression, loss of consciousness), on psychological health (e.g. anxiety, depression) and/or on social health (e.g. exclusion).
The reduction of risk is a public health strategy to prevent the harm associated with drug use, without judgement and with respect for the person who uses drugs. The reduction of risk is therefore complementary to prevention, which is intended to reduce the number of people who start using drugs, and to treatment, which aims to reduce or stop drug use.
The RoR is based on certain principles:
- Giving drug users the means to reduce the risks to which they are exposed
- Reaching out to drug users in their environment
- Involving drug users in their prevention and encouraging them to assume responsibility
- Changing social representations of drug users
- Raising awareness among professionals and improving the laws and systems in place
In concrete terms, RoR entails various measures:
RECREATIONAL


STREET


CUSTODIAL


CHEMSEX
In order to reduce the risk of HIV and Hepatitis C (HCV, cf. Module 6 for more details) infection among drug users, RoR promotes safer use, which entails the use of disposable single-use or individual drug paraphernalia, whether for injection or sniffing.
For consumption, this means using:
- Disposable, single use equipment
- Personal equipment
- New equipment

